It’s no secret that exercise is good for your heart—but did you know that may be especially true for women? A 2024 study from the Smidt Heart Institute at Cedars-Sinai shows that women who work out get more cardiovascular benefit out of each minute of moderate to vigorous exercise than their male counterparts do.1 During the study, the researchers analyzed data from 412,413 adults utilizing the National Health Interview Survey database. The participants—55 percent of whom were women—provided information on their leisure-time physical activity, including the frequency, duration, intensity and type of activity they engaged in. They found that the mortality and cardiovascular benefits among the men maxed out at 300 minutes of moderate to vigorous exercise per week. The women, on the other hand, got the same benefit from just 140 minutes per week. And the women who worked out more (up to 300 minutes per week) experienced even greater cardiovascular benefits. (Yes, we know that these gals may be more of an exception than the rule. That said, it’s good to know that, even if you aren’t a gym rat, you can tone up your cardiovascular system—as well as your biceps—by exercising about half as long as the men in your life.)
Why Your Heart Loves Exercise
Adding regular physical activity to your daily routine can improve your cardiovascular health in multiple ways:
- Improves overall cardiovascular health. Regular exercise can help strengthen the heart muscle, improves circulation, and lowers blood pressure, reducing the risk of heart attack and stroke.2
- Boosts VO2 Aerobic exercise improves VO2 max—the maximum amount of oxygen the body uses during intense exercise. A higher VO2 max level is an indication of better cardiorespiratory fitness and cardiovascular health.3
- Lowers cholesterol levels. Physical activity can raise levels of “good” HDL cholesterol and lower levels of “bad” LDL cholesterol, which can help prevent plaque buildup in the arteries.4
- Weight management. Exercise can help women maintain a healthy weight, reducing the risk of obesity-related cardiovascular conditions.5
- Reduces risk of diabetes. Regular physical activity can improve insulin sensitivity and help regulate blood sugar levels, lowering the risk of developing type 2 diabetes, which is a risk factor for heart disease.6
- Stress reduction. Exercise can help reduce stress levels and improve mental well-being, which can have a positive impact on your cardiovascular system.7
- Improves mood and sleep. Regular physical activity can boost mood, reduce anxiety and depression, and promote better sleep, all of which contribute to overall heart health.8,9
- Enhances overall fitness. Exercise can improve endurance, strength, and flexibility, making daily activities easier and reducing the risk of injury.10
Many of these benefits have been highlighted in two large studies. The Nurses’ Health Study has followed more than 70,000 female nurses for nearly half a century and found that those who engaged in regular physical activity had a significantly lower risk of developing heart disease compared to those who were inactive.11 The Women’s Health Initiative was even larger, involving more than 160,000 postmenopausal women. This ongoing study, which began in 1991, has consistently shown that participating in physical activity, including walking and vigorous exercise, significantly lowers the risk of heart attack and stroke in older women.12
The Best Workouts for Women
There are many great workouts for women, and the best ones for you will depend on your fitness goals and preferences. However you choose to move, there are three pillars that should be included in every woman’s fitness plan: Aerobics, strength training, and flexibility.
Here are some popular and effective workouts for women that can help to cover all your bases:
Cardio workouts. Running, cycling, swimming, and dancing are great aerobic options for increasing your heart rate, improving your overall cardiovascular health, and for burning calories. The American College of Cardiology notes that adding aerobics to your exercise plan can strengthen the heart and help it pump blood more efficiently.13
High-intensity interval training (HIIT). HIIT workouts involve short bursts of intense exercise followed by brief rest periods, making them efficient for burning calories and improving endurance, VO2 max, and the heart’s ability to pump blood throughout the body.14 As a bonus, HIIT workouts can be completed in a short amount of time. Plus, they can include either cardio, strength training, or a combination of the two.
Strength training. Weightlifting, bodyweight exercises, and resistance band workouts can help build muscle strength and tone your body. According to the American Heart Association, strength training also improves many risk factors for heart disease, including blood pressure, blood sugar, cholesterol, triglycerides, and body composition.15
Barre workouts. Barre classes combine elements of ballet, Pilates, and yoga to strengthen and tone muscles, particularly the muscles in your core, legs, and glutes. Barre workouts also offer notable cardiovascular benefits through a combination of low-impact, high-repetition movements that elevate the heart rate and engage multiple muscle groups. While not as intense as some cardio workouts, barre effectively improves endurance, stamina, and overall heart health.16
Pilates. This low-impact workout focuses on core strength, flexibility, and overall body alignment. More importantly, studies show that a regular Pilates practice boosts VO2 max levels.17
Yoga. Yoga can improve flexibility, strength, and mental well-being through a combination of poses, breathing exercises, and meditation. One large meta-analysis also found that yoga can improve heart rate variability (the variation in time between heartbeats, rather than the average number of heart beats per minute) and endothelial function. Yoga was also found to lower blood pressure, heart rate, oxidative stress, and inflammation—all risk factors for cardiovascular disease.18
Sticking with Your Exercise Routine
If you’re like most of us, you may embark on a fitness program full of motivation only to see your enthusiasm fade within a couple of weeks. Fortunately, there are some easy strategies that can help you stick to your exercise goals. First and foremost, choose activities that you enjoy. Whether it’s pickleball, Zumba, or something else entirely, you’re more likely to continue if your workouts are fun. You can also make your workouts more enjoyable by listening to your favorite tunes or podcasts. It’s also important to build accountability into your workouts, especially when you’re just beginning. Exercising with friends or working with a qualified trainer can help you stick to your fitness plan. Finally, mix up your activities to keep things interesting.
Optimize Your Heart Health Even More
Increase the heart-healthy benefits of regular exercise even more by adding an Aged Garlic Extract (AGE) supplement to your workout routine. A number of studies clearly show that AGE helps to reduce blood pressure and cholesterol while slowing the accumulation of calcium deposits and plaque in arteries.19,20 But supplementing with AGE can also support your fitness goals. A recent randomized, double-blind, placebo-controlled trial found that a daily dose of AGE improved aerobic fitness in a group of middle-aged recreational endurance athletes. Those taking AGE experienced improvements in their VO2max and aerobic power, while increasing the amount time before experiencing muscle fatigue. Plus those who supplemented had less muscle soreness and faster post-workout recovery time. The participants in the placebo group didn’t experience any of these benefits.21
Go Girls!
Adopting a regular fitness routine can help you look and feel your best while giving your whole cardiovascular system a boost. But to reap all the benefits physical activity can provide, it’s important for women to engage in a combination of aerobic exercise, strength training, and flexibility exercises. Adding AGE to your exercise journey can enhance your cardiovascular health and fitness results even more! Just remember to consult with your healthcare provider before starting a new exercise routine, especially if you have any existing health conditions.




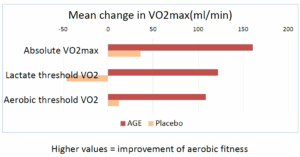 These benefits weren’t seen in those taking the placebo. The participants taking AGE also had a lower risk of cardiovascular disease compared to those in the placebo group.
These benefits weren’t seen in those taking the placebo. The participants taking AGE also had a lower risk of cardiovascular disease compared to those in the placebo group.